What is an inherited retinal disease?
An inherited retinal disease (IRD) is a condition caused by a genetic anomaly that leads to loss of vision and in some cases, legal blindness. It is rare for an IRD to cause complete, black-blindness.
Inherited retinal diseases are also known as inherited retinal dystrophies or inherited retinal degenerations.
There are over 20 types of inherited retinal diseases. Depending on the disease, you may have vision loss at birth, or it may occur later in life.
What causes an inherited retinal disease?
Genetic error
An inherited retinal disease is caused by a variation in your genetic code or DNA.
You can think of DNA as a recipe book, which contains all the instructions needed for your body to make the proteins to survive and thrive. Proteins are important as they provide cell structure, function and regulation of the body. In genetic diseases, there is an error in one of the recipes, which can lead to disease.
In IRDs, the genetic error usually results in an abnormality of the photoreceptor cells in the retina. The retina is the light-sensitive tissue at the back of the eye that senses and transmits light signals to the brain through the optic nerve to form images, enabling people to see.
Over 300 IRD associated genes
Researchers have found over 300 genes that cause IRDs. 1
Some IRDs, such as choroideremia or juvenile X-linked retinoschisis, are caused by one or only a small number of genes (known as a “monogenic” disease). Other diseases can be caused by many different mutations in many different genes. For example, over 70 different genes have been identified that can cause retinitis pigmentosa. Some gene anomalies cause more severe inherited retinal diseases than others.
60% successfully diagnosed
Currently, we are only able to find the causative gene mutation for about 6 in 10 people. This is because we still do not know all the genes that cause IRDs and, in some cases, our testing is not sensitive enough to detect certain changes in the genetic information.
However, researchers are working on more sensitive ways to examine a person’s genetic code in more detail, which should improve this number over time.
Inheritance patterns
The way that each IRD is passed from generation to generation (inheritance pattern) can be different in each family.
- You may have a strong family history and know a family member with the condition.
- Or you may be the first one in your family to be diagnosed.
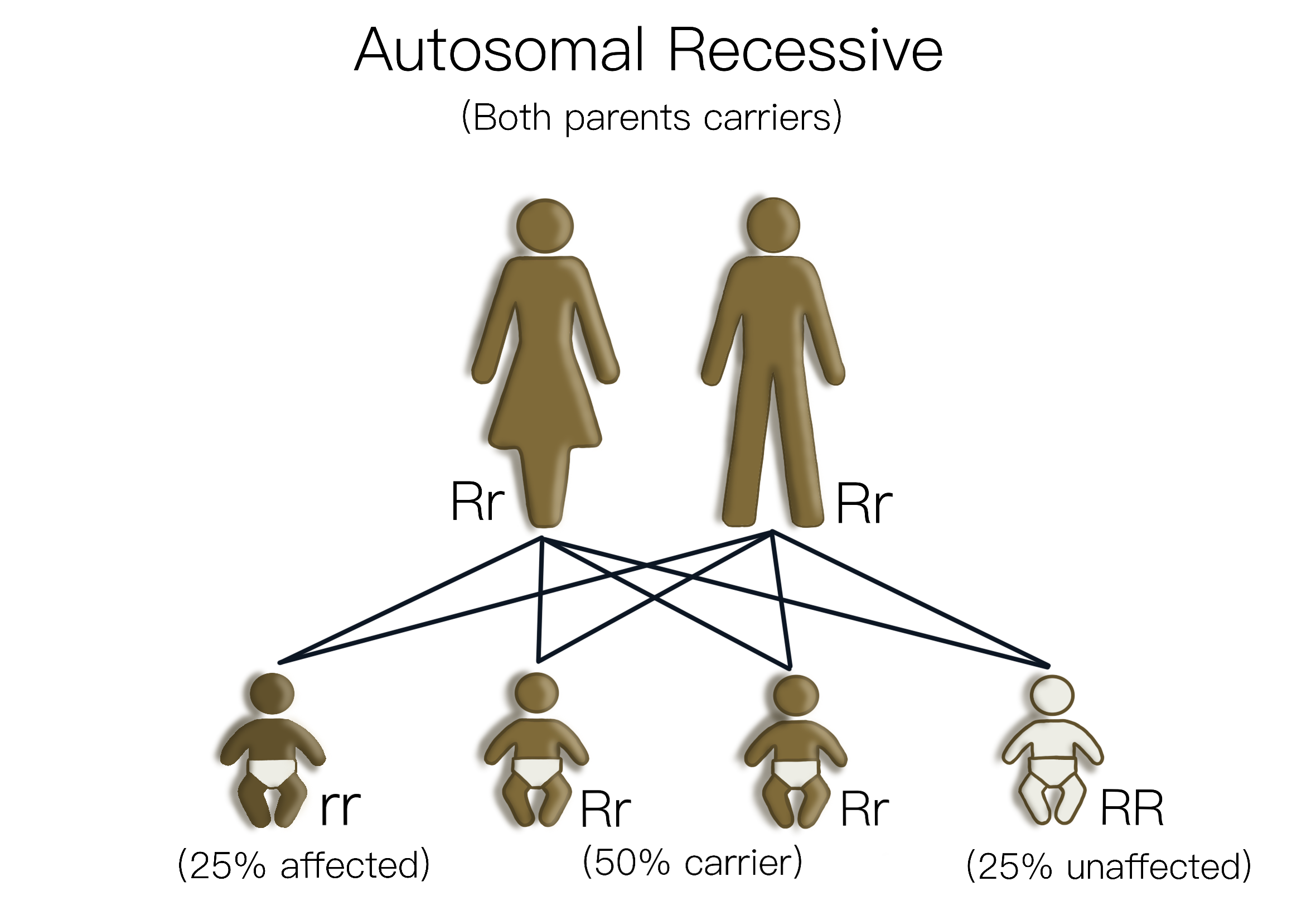
The different inheritance patterns of IRDs mean that there are different chances of children inheriting a condition, depending on the pattern. For example, recessive conditions can skip generations, whereas dominant inheritance is more likely to be present in most generations. In addition, it is possible for a person to develop an entirely new genetic mutation – this is known as a “de novo” gene variant. For more details, refer the “Inheritance Patterns” section.
Syndromic IRDs
In most people, IRDs only affect the eyes. However, some types are linked with other health issues, such as Usher syndrome (which also affects hearing). 2
How many people live with an inherited retinal disease?
It is estimated that around ~ 1 in 1380 people are living with an IRD, which is ~ 19,000 people in Australia. 3 4
IRDs are currently known to be:
- the leading cause of blindness in working age adults and
- the second leading cause of blindness in children in Australia (following cerebral visual impairment). 5
Total estimated lifetime cost was $5.2 million per person with an IRD, of which 87% were societal and 13% health care costs. 6
Disease progression
IRDs can affect individuals of all ages and genders and can progress at different rates. Some may be born with or experience vision loss in infancy or early childhood. Some may experience a gradual loss of vision later in life.
The prognosis of an IRD also varies – some people will lose all vision, whilst others will have more mild disease.
Your ophthalmologist may be able to give you some indication of the expected future for you, based on your clinical presentation and genetic testing, but this is not an exact science. Sometimes, it can be unpredictable as to how the disease will proceed.
Common symptoms of IRDs
Each IRD is different, but common symptoms may include:
- Low vision at night, or in dim or dark settings
- Loss of central and peripheral vision
- Sensitivity to light, glare and difficulty in bright light
- Farsightedness or shortsightedness (requiring glasses or contact lenses)
- Blind spots
- Colour differentiation difficulties or not seeing all colours
- Uncontrolled eye movements (nystagmus)

Vision loss can vary between different IRDs
In some conditions, only the central vision is lost, while others lose peripheral vision first, with a slow progression into the central vision areas. Some people will only ever have mild vision loss, whilst others can progress to lose all vision, also known as “no light perception” or “black-blindness”.
At some stage, people with an IRD may be told that they are “legally blind”. This term has slightly different meanings in different parts of the world. In Australia, to be classified as legally blind a person’s central vision must be below 6/60 on a visual acuity chart (this is typically the top line on a standard letter chart) and/or they have tunnel vision of less than 10 degrees remaining. Legal blindness allows people to access certain government resources, but does not mean that all sight has gone.
There have been numerous research studies over decades to try and learn what the prognosis is of certain subtypes of IRD, so your doctor will be able to give some indication of the expectations for you. However, it is important to note that no one can predict the future, and no one will be able to tell you exactly what your journey will be.
Obtaining a confirmed diagnosis through genetic testing is the only way to verify the exact gene anomaly(s) that is the underlying cause of an IRD. 7
How do I know what type of IRD I have?
Difficulty in diagnosis
Usually when you are first diagnosed with an IRD, the name of the disease used can be variable, and sometimes change from doctor to doctor. This is because IRDs are complex to diagnose, with many different genes and clinical presentations.
Molecular diagnosis through genetic testing
As mentioned above, there are over 300 known IRD genes. However, there is a lot of overlap between the genes, so that some different genes cause changes to the retina that look the same. Conversely, sometimes the same gene can present differently in different people. The gold standard is called a “molecular diagnosis”, which is when you complete genetic testing and receive a report on the genetic cause of your IRD.
An example of the complexity of naming IRDs is the IRDs caused by the gene RPE65. This is the gene for which a treatment exists, the gene therapy Luxturna®. The gene RPE65 can cause slightly different clinical presentations, which can be called retinitis pigmentosa (RP) or Leber congenital amaurosis (LCA). To reduce confusion, sometimes doctors and researchers will just refer to the condition by the gene name; in this case, that would be RPE65-associated retinal degeneration.
What treatments are currently available?
Luxturna
In Australia, there is currently only one regulatory-approved treatment for an IRD – a gene therapy called Luxturna®, for those related to mutations in the RPE65 gene. As mentioned above, associated IRD conditions may include retinitis pigmentosa (RP) or Leber congenital amaurosis (LCA)
Luxturna® was approved by the Australian Therapeutic Goods Administration (TGA) in 2020 and is currently available at two treatment sites – the Sydney Eye Hospital and the Royal Victorian Eye and Ear Hospital.
Idebenone (internationally only)
Internationally, patients with Leber hereditary optic neuropathy (LHON) can access an antioxidant medication called idebenone (Raxone®). In LHON, people present with sudden vision loss, and the use of oral idebenone 900 mg/day for 24 weeks has been shown to have persistent beneficial effects in preventing further vision impairment and promoting vision recovery. 8
Idebenone is not currently available in Australia but has received regulatory approval in Europe and Israel.
Emerging treatments
In addition to these options, a number of emerging treatments are currently in the research and development pipeline. These include gene therapy, stem cell therapy, optogenetics, pharmaceutical compounds and vision prostheses. For more information, see the “Emerging treatments” section of this website.
There is no guarantee that these treatments will become available for people with an IRD, as stringent clinical trials must be performed first to show safety and efficacy.
If you are interested in registering your interest in participating in clinical trials, you can register your interest through IRD registries. Your ophthalmologist will also be able to provide you with information about what treatments may be an option for you in the future.