15 October, 2025 | Author: GenIMPACT: Centre for Economic Impacts of Genomic Medicine, Macquarie University
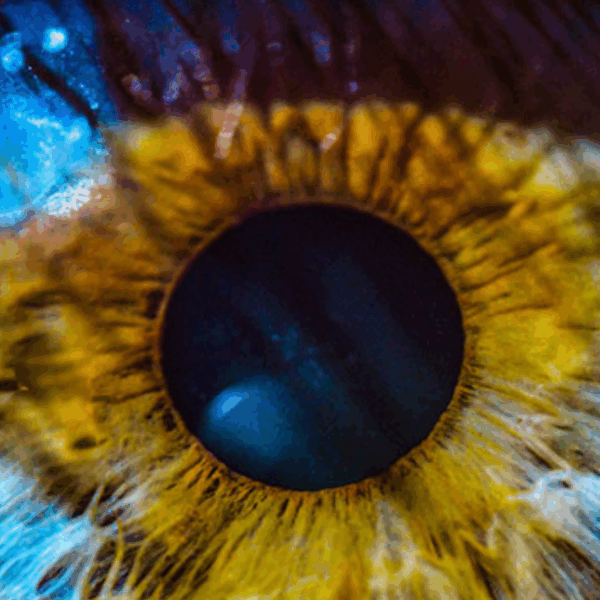
Visual impairment resulting from inherited retinal dystrophy (IRD) has substantial economic and psychosocial impacts on affected individuals, their families, and large financial costs to the government. However, the full extent of these impacts has yet to be measured.
For many individuals and their families, the genetic cause of their disease is unknown, leaving them with feelings of uncertainty about their future and the future health of their children. Genomic sequencing combined with expert review at multidisciplinary team (MDT) meetings has the potential to improve diagnostic rates, reduce economic and emotional burden, and open the door to emerging genetic therapies.
Aim of the study
The EPIC-Vision Study aims to understand and quantify the economic and psychosocial challenges faced by families with IRD. It will also model the potential economic and social benefits of genome sequencing, multidisciplinary team review, functional genomic studies and therapies in this population.
The findings will help to improve support systems for families affected by IRD and those who undergo genetic testing. They will also highlight the health and social costs of IRD at all stages of patients’ lives.
The EPIC-Vision Study is led by researchers at Macquarie University, in collaboration with clinicians, researchers and health professionals from New South Wales, Victoria, Western Australia and New Zealand. Supported by new funding and in-kind support from an NHMRC Partnership Project and industry, clinical service providers and government, this study builds upon a prior NSW-based pilot project.
Who is eligible to participate?
Adult (18+ years) participants or primary carers of children and adults with the following diagnoses are eligible to participate:
- Stargardt disease
- Usher Syndrome
- Leber congenital amaurosis (LCA)
- Retinitis pigmentosa
- Choroideremia
- Cone-rod dystrophy (CRD)
- X-linked retinoschisis
- Cone dystrophy and achromatopsia
- Leber hereditary neuropathy
Recruitment will take place across NSW, VIC, WA and New Zealand. Participants must live in Australia or New Zealand and speak English.
What does participation involve?
Adult patients and carers in the study will be asked to complete a 60–90-minute questionnaire with a researcher and a similar follow-up survey 12 months later . The surveys can be completed in person, over the telephone, or via an online video call. Questionnaires for children and partners will take approximately 10-20 minutes and will be completed during the same appointment.
Participants will also be asked to consent to allow access to their medical expenses records (e.g. hospital and Medicare records) which will be linked with their survey responses. This will provide a thorough record of the healthcare services the participant has used.
Why the study matters
The findings from this research could potentially improve the services and support for families affected by vision impairment. In particular, the study aims to:
- Address critical knowledge gaps regarding the economic cost-effectiveness of genomic testing in IRDs;
- Assess the broader impacts of diagnosis, including effects on reproductive decision-making and emotional wellbeing;
- Estimate for the impact of access to precision medicine on public health and social welfare systems; and
- Support the development of targeted interventions and genetic therapies by identifying the needs and priorities of affected families
While there may be no direct or proven benefits for participants, many find that sharing their experiences provides them an opportunity for their needs to be recognised and value the opportunity to contribute information that may support submission to seek funding to provide improved services to families affected by IRD.
Who is conducting this research?
The study is being conducted by researchers, clinicians and health professionals across NSW, VIC, WA and New Zealand.
These organisations include: Macquarie University, University of Sydney, University of Melbourne, University of Western Australia, University of Auckland, Lions Eye Institute, NSW Agency for Clinical Innovation, The Royal Australian and New Zealand College of Ophthalmologists (RANZCO), South Eastern Sydney Local Health District (SESLHD), Sydney Children’s Hospitals Network, Health New Zealand – Te Whatu Ora Te Matau a Māui Hawke’s Bay, The Royal Victorian Eye and Ear Hospital, The SA And GJ Ombler Charitable Trust, Illumina, Johnson & Johnson Innovative Medicine, Nacuity Pharmaceuticals, Inc., PYC Therapeutics, Belite Bio, Cure Blindness Australia Inc, Genetic Alliance Australia, Guide Dogs NSW/ACT, Retina Australia, Vision Australia.
The project is supported by a National Health and Medical Research Council (NHMRC) Partnership Projects Grant: APP2027453 “Translation of precision medicine into clinics for genetic blindness: from diagnosis to clinical management and therapies” (led by Macquarie University).
Recruiting clinics:
- NSW – Ophthalmic Clinics at Sydney Eye Hospital, Save Sight Institute and The Children’s Hospital at Westmead
- VIC – The Royal Victorian Ear and Eye Hospital, The University of Melbourne, Centre for Eye Research Australia
- WA – Lion’s Eye Institute, Perth Children’s Hospital
- New Zealand – Greenlane Clinical Centre, Eye Department, Te Toka Tomai
If you are a patient at any of the above recruiting clinics and are interested in participating in the study, please discuss with your ophthalmologist.
https://retinaaustralia.com.au/the-economic-and-psychosocial-impact-of-caring-for-families-affected-by-visual-impairment-epic-vision-study/
Other Blogs

Autosomal Dominant Optic Atrophy Webinar
Supporting people affected by mitochondrial disease Many types of mitochondrial disease (mito) can lead to progressive vision loss and blindness....
World Research Summary by Dr Catherine Civil
Hot Off The Press A very Happy New Year to you all, and may 2026 bring us another step closer to...

World Geographic Atrophy Day 2025
A New Era of Hope for Vision Preservation Geographic Atrophy (GA), a progressive and irreversible form of advanced age-related macular degeneration (AMD), has long been a...
