21 September, 2023
This is a summary of the webinar held on Tuesday 8th August, 2023, featuring two of Retina Australia’s recent research grant recipients. You can also view a video recording of this event here.
RNA base editing strategies as potential therapeutic of inherited retinal dystrophies
Associate Professor Rick Liu from the Centre for Eye Research in Melbourne spoke about his team’s work on RNA base editing and its potential as a therapeutic for inherited retinal disease (IRD).
While Luxturna has been highly successful in treating Leber’s Congenital Amaurosis (LCA) by introducing a normal version of the RPE65 gene into the eye using an adeno-associated virus (AAV) vector, treatment for many other IRDs will not be possible using this technology, as around 45% of the up to 300 different genes that cause IRDs are too large to be delivered by AAVs.
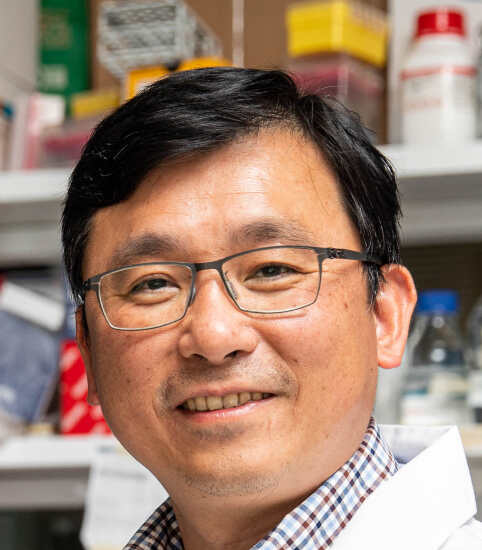
This investigation explored how the latest gene editing technology might be able to be used instead. Conventional CRISPR-Cas gene editing technology provides an opportunity to change sections of mutant DNA, but again, in many cases it is too large to be introduced into the eye using an AAV, and it can be inefficient, altering other components as well as the target area.
Thus, Associate Professor Liu and team sought to revolutionise gene therapy for IRDs using another gene editing approach, RNA base editing. RNA base editing is designed to correct single nucleotide base mutations (point mutations) in RNA transcripts, the messenger transcribed from genes to make proteins. Since more than half of the mutations that cause IRDs are caused by single nucleotide base mutations, this approach may address the current unmet need for treating a broad spectrum of IRDs.
In this project, the team first compared two recently developed RNA base editing systems, CRISPR-Cas RNA base editor and CRISPR-Cas-inspired RNA targeting system (CIRTS), and effectiveness of these systems for correcting single nucleotide base mutation was investigated using a fluorescent reporter system. In this case the CRISPR-Cas RNA base editor was able to correct the mutation and recover fluorescence in more than 90% of the cells, while the CIRTS system was less effective.
Next, the team performed the proof-of-concept study by correcting the single base mutation on one of the well-known IRD genes, RPE65. Again, the results show that the CRISPR-Cas RNA base editor can effectively correct the single nucleotide base mutation on the RPE65 gene and restore the protein expression in cultured human retinal pigment epithelium cells. The study has been moved forward to in vivo testing to evaluate the CRISPR-Cas RNA base editor in an IRD mouse model (Rd12) carrying the Rpe65 gene mutation similar to the human LCA disease.
Moreover, the team are also working on another IRD mutation in the USH2A gene, in the retinal cells that occurs in Usher Syndrome. Using the CRISPR-Cas RNA base editor in this case led to a correction rate of up to 65%, but it also included some unwanted off-target changes. However, with some modification of the guide RNA and using another new technology called domain-inlaid CRISPR-Cas RNA base editor, many of these unwanted changes could be minimized. Overall, the results are very promising.
While future work in this area will require developing safer RNA base editors, improving delivery efficacy into as many retinal cells as possible, and working directly with patients, these results have demonstrated the feasibility of using this genetic tool to address different IRD mutations. With development of further genetic technologies, more tools will be available to address different types of IRDs better and prevent vision loss in these patients in the future.
You can read the full details of this research project here.
Neuroprotective effect of SAHA in Retinitis Pigmentosa. Do time and frequency matter?
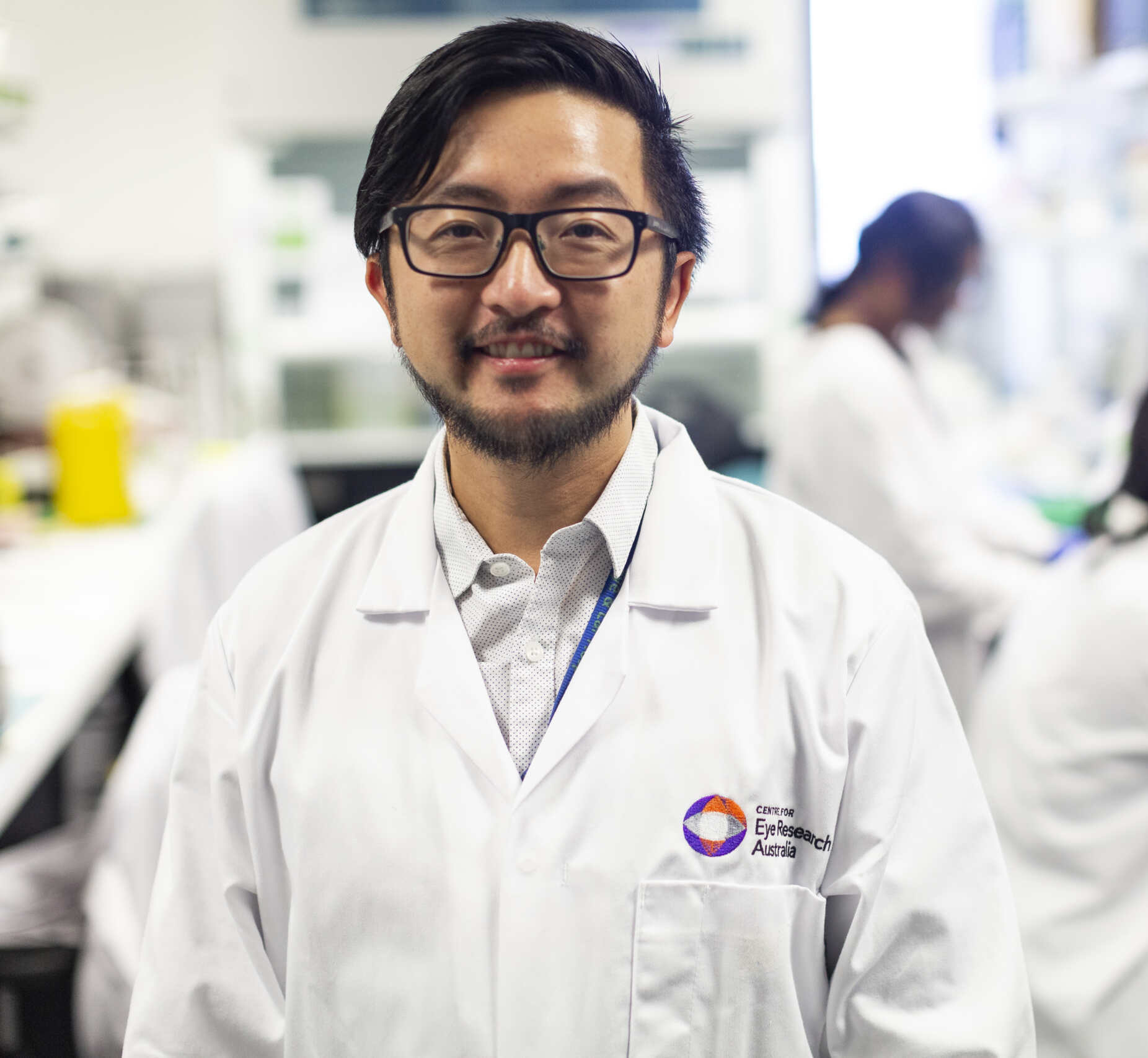
Our second speaker was Annie Miller, a PhD candidate from the Lions Eye Institute in Perth. She presented the results of work done looking at the suitability of a gene independent treatment for Retinitis Pigmentosa (RP).
Currently these solutions are being tested in the laboratory rather than being available as actual treatments. They include things such as retinal prosthesis, cell therapies and pharmaceuticals that can prevent the cell loss that happens in these diseases.

In RP, the rod and cone cells die due to a number of different processes, and once they are dead they can’t regenerate. One of the causes of these deaths is thought to be the accumulation of a molecule called cGMP, which leads to the accumulation of other molecules through a cascade effect and results in cell death. One of these molecules is called HDAC or histone deacetylase. It is thought that an increase of HDAC in the cell due to the RP mutation can lead to the cell death.
This project focused on the development of a broad treatment approach that could be used on RP patients by investigating the effect of an FDA-approved HDAC inhibitor (SAHA) to protect photoreceptor cells, especially cones, from degeneration in two mouse models of RP, the autosomal recessive model (rd1) and the autosomal dominant model (RhoP23H/+).
The intraocular administration (via injection to the eye) of SAHA to the mice was tested once the photoreceptors had started degenerating but some were still present. In the rd1 mouse model, which degenerates very quickly, results showed that the drug did rescue some of the peripheral photoreceptor cells but did not rescue the central photoreceptors, likely as they were too far degenerated already. While SAHA potentially has a net protective effect in the retina of these mice, the effects of the drug seem to wane over time.
The work done in the RhoP23H/+ model of RP is still preliminary with their lab group currently working on more experiments. However, their preliminary data showed positive results, showing that administration of SAHA at 2 months old allows for a significant protection of the photoreceptors four days after treatment.
Future work will focus on quantification of cone numbers after treatment, and assessing whether multiple injections of SAHA will increase the period of effectiveness of the drug. The team is also planning to study the neuroprotective effects in other mouse models of IRDs, e.g. Achromatopsia models, as HDAC has been implicated in a number of different IRDs.
You can read the full details of this research project here.
https://retinaaustralia.com.au/rna-based-gene-editing-and-testing-of-a-gene-independent-treatment-strategy/
Other Blogs
Research Grant Impact Highlight: Associate Professor Raymond Wong
Associate Professor Raymond Wong, from the Centre for Eye...
Research Updates on Inherited Retinal Diseases: ARVO 2025 Summary
For those living with inherited retinal diseases (IRDs), and...

New Research: The burden of X-linked retinitis pigmentosa (XLRP) on patient experience and patient-reported outcomes
X-linked retinitis pigmentosa (XLRP) is considered one of the...
